People who work in hospice care understand that, at its core, it is the lived experience of patients and their families during some of life’s most vulnerable moments. As regulatory expectations rise and patient-centered care becomes the standard, hospice providers should proactively influence the quality measures that shape outcomes, perceptions, and reimbursement.
Key hospice quality and patient survey measures are shifting the focus to patient-centered care, and there are numerous practical strategies to improve care and, consequently, measures so you can track the correct things to make informed moves toward improvement.
Actionable Strategies to Improve CAHPS Scores
For seasoned hospice providers, improving quality outcomes is about delivering quality care. However, measuring it and ensuring the outcomes align with the care delivered is best understood through metrics and CAHPS scores. The CAHPS Hospice Survey offers critical insight into how well your team supports patients and families across the end-of-life journey.
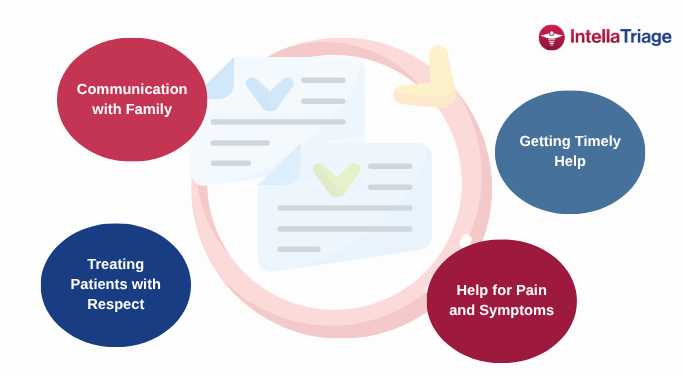
Below, we review four high-impact CAHPS domains that are significantly influenced by after-hours care. These are not just moments in time but opportunities to improve survey results and, consequently, patient satisfaction. The strategies provided include special considerations for after-hours care and are designed to help providers deliver quality and compassionate care, thereby enhancing the patient experience.
1. Communication with Family
Importance of regular, clear, and compassionate communication
Why It Matters
Families are often the voice of the patient, and how you communicate with families defines the entire hospice experience. CAHPS questions assess whether hospice staff kept families informed, listened carefully, and explained things clearly.
Actionable Strategies
- Enhance Patient Engagement Services. Proactively establish a patient engagement plan of proactive outreach and check-in calls to foster stronger patient relationships and deeper insights into patient status. This proactive approach enhances trust and reduces the need for calls during off-hours.
- Standardize Family Conferences. Ensure that weekly interdisciplinary team (IDT) family calls or meetings, especially for complex cases, follow consistent patterns and allocate time for clear and concise communication of care plans and changes – including feedback loops to ensure understanding.
- Have Communication Scripts Available for Sensitive Conversations – But Encourage Individualized Conversations. Developing team-wide scripts or communication guides can promote consistent language when discussing changes in conditions, medications, or care goals. However, prescripted responses significantly cut into empathy and compassion. Providing staff with supportive “scripts” that smooth conversation can be helpful, but training that helps them treat each patient as an individual is the best.
- After-Hours Tip:
- Real-time access to care records. Ensure triage nurses have access to clinical updates and clear protocols for conveying information compassionately at night. A calm, informed tone during a 2 a.m. call goes a long way.
- Anytime Access to Nurse Support: Partner with services like IntellaTriage to provide families with direct access to licensed nurses at any time, thereby reducing anxiety and improving satisfaction.
2. Getting Timely Help
Ensuring responsiveness to patient needs
Why It Matters
CAHPS scores drop sharply when families feel their loved ones didn’t get help quickly. That impact can be felt especially at night or over weekends when concerns about lack of nurse access exacerbate feelings of helplessness and vulnerability. This domain assesses whether the hospice team responded promptly when the patient required assistance.
Actionable Strategies
- Commit to a Timely Callback Policy. Set a triage goal: all calls answered or returned within x # of minutes. Monitor and track response times and address outliers quickly.
- Create a Symptom Triage Protocol. Use a standardized symptom urgency grid for calls and after-hours triage to efficiently and safely prioritize patient needs.
- After-Hours Tips.
- Measure Your Calls. Audit weekend call volumes and response times monthly. If family members report long waits, consider expanding peak-time staffing or rotating clinicians for on-call support.
- Adopt a Nurse-First Triage Model. Implementing a nurse-first approach, where patients speak directly with a licensed nurse (IntellaTriage connects patients to a nurse within an average of 38 seconds), can significantly reduce emergency room visits and enhance patient satisfaction. This model ensures that patients receive prompt and appropriate care, even after hours, which can substantially improve their experience and CAHPS scores.
3. Treating Patients with Respect
Training for empathy, cultural competence, and honoring autonomy
Why It Matters
This CAHPS measure assesses whether the hospice team treated the patient with dignity, clearly explained care options, and respected their values and preferences.
Actionable Strategies
- Ongoing Empathy & Cultural Sensitivity Training. Include real-world case studies and roleplay during team meetings to reinforce respectful communication and culturally aligned care.
- Document and Honor Patient Preferences. Include patient values and spiritual needs prominently in the care plan and review them at every Interdisciplinary Team (IDT) meeting. For example, note if a patient prefers music, prayer, or quiet during visits.
- After-Hours Tip:
- Understand Patient Wishes. Ensure after-hours staff can access advance directives and documented patient wishes. A misstep in honoring final preferences can be deeply distressing to families.
- Maintain Consistent Care: Train after-hours staff to provide compassionate and culturally competent care, maintaining the same standards as daytime staff.
4. Help for Pain and Symptoms
Importance of effective pain and symptom management
Why It Matters
Uncontrolled pain or distress is one of the fastest ways to erode trust. This domain asks families if the hospice team helped with pain, shortness of breath, anxiety, and other symptoms promptly and effectively.
Actionable Strategies
- Initiate Frequent Symptom Checks. Create a symptom review checklist to be used at every visit—even virtual check-ins. Set a standard for reassessment within 1–2 hours after intervention.
- Empower Nurses with Protocols
- Create standing orders or rapid-response protocols for urgent symptoms (e.g., pain, agitation, dyspnea), allowing nurses to intervene promptly—without delays for physician approval.
- Use Non-Pharmacologic Support
- Train aides, social workers, and chaplains in simple comfort measures, such as massage, guided imagery, music, or breathing techniques.
- After-Hours Tip:
- Equip triage nurses with “pain rescue packs” protocols and empower them to dispatch PRN medications or make home visits when needed. A nurse visit at midnight to manage pain can prevent unnecessary ER transfers and elevate family trust.
- Implement a Nurse-First Triage System: Having licensed nurses available after hours to assess and address symptoms can prevent unnecessary hospital visits and enhance patient comfort.
Final Thought: Every Patient Contact Counts
Each phone call, nurse visit, and quiet moment of presence is a quality measure in action. For seasoned hospice providers, the challenge is no longer understanding what good care looks like, but instead, it’s delivering it consistently, including after hours.
By refining communication, strengthening responsiveness, and putting patient values at the center, you both boost your CAHPS scores and affirm a key aspect of hospice care: compassion, dignity, and comfort when it matters most.
Quality is a promise. Let’s keep it day and night, weekday, or weekend.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
Home health and hospice leaders know the strain of delivering quality care 24/7 with shrinking staff, rising patient volumes, and growing oversight. One strategy many haven’t fully leveraged yet is after-hours triage. A nurse-first triage model is about more than answering calls. Outsourcing your nurse triage function is a strategy that saves money, strengthens staff [...]
As post-acute care evolves under the weight of rising patient volumes, persistent staffing shortages, and the increasing complexity of care at home, one thing has become undeniably clear: nurse-first triage is an invaluable piece of the care-at-home puzzle. At IntellaTriage, we've spent the last 16 years proving that. From our earliest days in 2008, our [...]
In hospice and home health, nurses are the lifeline of care. But with higher acuity in the care-at-home patient population, mounting documentation demands, and a growing aging population, field nurses are stretched thin. The stakes are high for today's care delivery, but for the future of the profession itself. Persistent Post-Acute Trends Worth Paying Attention [...]