Starting September 30, 2025, the Centers for Medicare & Medicaid Services (CMS) will roll out the HOPE (Hospice Outcomes and Patient Evaluation) assessment tool, a game-changer in patient satisfaction surveys and quality reporting for hospices. Replacing the current HIS, CMS designed this new tool to provide a more comprehensive picture of each hospice patient’s journey, from admission to critical touchpoints during care.
The HOPE tool refines the data collection process and emphasizes timely follow-ups, symptom management, and consistent patient care. Here’s what you need to know about the changes and how to prepare your hospice agency for success.
Why the HOPE Assessment Tool Matters
The HOPE tool represents a significant shift in how hospice care captures patient satisfaction scores and quality measures during end-of-life care. By introducing these new standardized data elements, CMS aims to improve the quality of care via deeper understanding of patient care needs.
- Enhanced Focus on Patient Care: The HOPE data elements track patient-level details from admission and other critical timepoints, offering a clearer picture of patient experiences and outcomes throughout their stay.
- Impact on Quality Scores: Data collected from the HOPE tool will contribute to future CMS Hospice Quality Reporting Program Quality Measures, directly influencing HCAHPS and overall patient satisfaction scores. The first two new data elements evaluated for quality measures (as per FY 2025 Hospice Final Rule) are Timely Follow-up for Pain Impact and Timely Follow-up for Non-Pain Symptom Impact.
Key Changes and Requirements
- New HOPE Update Visits (HUVs):
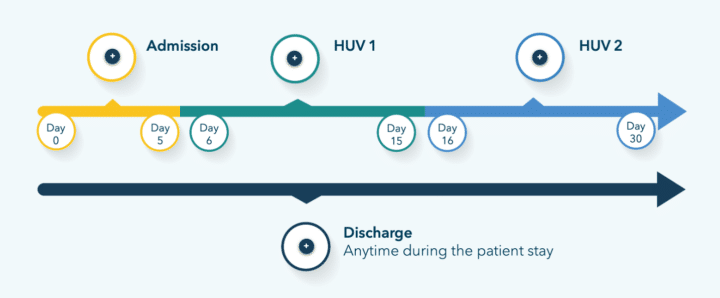
- In addition to the minimum Admission and Discharge data, hospices must conduct visits (HUVs) during days 6–15 and 16–30 of a patient’s episode if they remain on service.
- These visits ensure continuity of care and thorough documentation, aligning with HOPE’s goals of tracking patient experiences more closely.
- Most agencies already perform these visits, so likely the significant change here will be in the reporting, not the performance, of these visits.
- New Symptom Follow-Up Visits (SFVs):
- Must be completed within two calendar days if a pain symptom is reported as 2. Moderate or 3. Severe on the Symptom Impact data element.
- An RN, LPN, or NP can perform these visits (if documenting as a nurse). However, MDs and DOs are not eligible to conduct them.
- Agencies must ensure SFVs can be performed on weekends to remain compliant.
- Timely Data Submission:
- HOPE-Admission and HOPE-Discharge records must be submitted to and accepted by CMS within 30 days of completion.
- HUV records are within 30 days of the visit, as are SFV records, but you can consider submitting them together.
- CMS offers a web-based course which contains this great timeline image for reference.
How to Prepare Your Agency
- Coordinate With Your Software Providers: Ensure your EMR and data collection software systems are ready to handle HOPE survey requirements. Your software providers must align their systems with CMS’s timelines and data submission rules.
- Train Your Team: Educate your staff on the new HOPE requirements. Education should include:
- Submissions and visit timelines for HOPE update visits (HUVs) and symptom follow-up visits (SFVs).
- Documentation standards, especially for patient exclusions – when patient follow-up cannot occur for reason beyond your control. (During a recent CHAPCA conference education session, Judy Lund Pearson suggested, “Document the heck out of your patient exclusions.” We couldn’t agree more.)
- Maintain a minimum goal of a 90% data submission threshold for compliance.
- Try sharing this video.
- Prioritize Symptom Follow-Ups: Timely symptom follow-ups and accurate documentation are critical. To meet the two-day requirement, develop workflows that enable swift responses, even on weekends.
- Leverage QAPI Programs: The data collected through HOPE supports quality improvement initiatives. Use this information to refine your hospice plan of care and strengthen your Quality Assessment and Performance Improvement (QAPI) efforts.
Final Thoughts
The HOPE tool is more than a new regulatory requirement. Consider it an opportunity to improve patient care and satisfaction while streamlining processes. Start preparing now by collaborating with your software providers, training your staff, and ensuring compliance with the new requirements.
With the right preparation, your agency can not only meet CMS’s expectations but also deliver exceptional patient experiences, positively influencing patient satisfaction scores and overall outcomes.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
There’s a quiet cost in hospice and home health that rarely appears on a balance sheet. It’s the cost of unresolved work. The chart that couldn’t be closed timely. The family call that didn’t quite feel finished. The repeat caller who calls are not being linked to each other. The uncertainty that follows a nurse [...]
Patient needs don’t end at the close of business. But many care delivery systems still do. In home health, hospice, and palliative care, patients and caregivers experience care as continuous. Symptoms evolve unpredictably. Questions arise outside scheduled visits. Yet many organizations still rely on fragments models that operate after-hours triage care as separately from daytime [...]
Patient needs don’t end with the workday and care shouldn’t either. But sustaining continuous care across all hours is far from simple. The real challenge for home-based care organizations is not in recognizing this truth, but rather in designing systems that can support continuous, clinically sound care across all hours and the full episode of [...]