Many hospice organizations are experiencing a growing need for insight into what occurs after hours when they “flip their phones” for the day but lack after-hours action plans. 75% of the week occurs after you shut your agency doors, impacting multiple facets of your operations – especially your workforce. According to a recent 2022 Hospice News Outlook Survey and Report, over 67% of the hospice care professionals surveyed indicated that staffing would be their greatest non-COVID-related challenge this year. Learn how CommonSpirit Health at Home (CHI Health at Home) optimized its workforce using analytics, adjustments, and an action plan. That plan included outsourcing triage to IntellaTriage.
Analysis and Adjustments in After-Hours
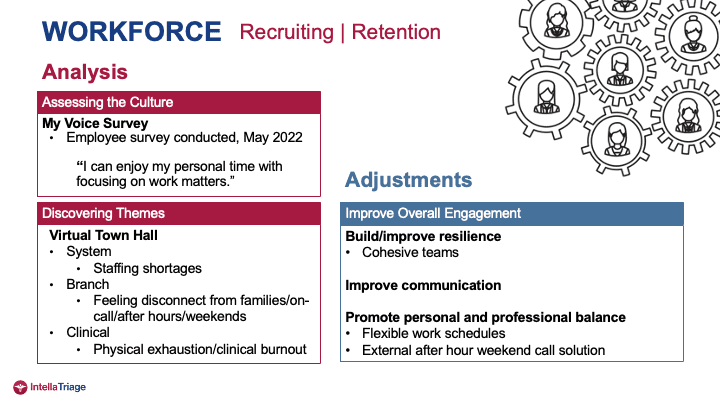
CHI Health at Home partnered with IntellaTriage in June 2022 for after-hours home health and hospice coverage. The journey began several years before COVID. Pre-COVID, CHI Health at Home company-wide town halls and My Voice surveys uncovered the taxing effort it took for staff to support patients after hours and on weekends and then come to work refreshed. It was becoming increasingly difficult for staff and management to be on call at night and do well during the day or to find a nurse or clinician to work after hours and on weekends. Feedback uncovered themes that led to adjustments surrounding how to improve resilience. They asked questions such as:
- How do we prioritize getting nurses time off, reducing their workload, and the stress of that? How can we improve communication with our staff?
- Does information about a patient’s needs get passed on from staff member to staff member timely and appropriately? How does it occur?
- What does all of that look like?
CHI Health at Home executives began to refer to and prioritize personal and professional balance versus work-life balance. They created an action plan identifying where change was needed and where they could improve quickly at a system, branch, and clinical level. They launched a partnership with IntellaTriage.
Staffing shortages were the number one issue at CommonSpirit town halls. They needed to find a solution for our employees feeling disconnected from their families: after hours and on weekends, stepping out of events to take a call or make a visit. CHI Health at Home discovered that the turnover rate was increasing due to physical exhaustion and clinical burnout, especially if the weekend nurse went from Friday to Monday.
“The 63 hours from 5:00 PM on Friday to 8:00 AM on Monday is when the hospice is most vulnerable (after-hours weekdays as well). The weekend is when the nursing staff tries to disconnect and enjoy personal time without focusing on work matters. Providing the staff with the confidence to put their phone down and enjoy their time and know that their patients were taken care of – that was the struggle.” – Lisa Schmitz, Regional Vice President of Operations, CommonSpirit Health at Home.
After-hours Action Plans
CHI Health at Home took steps to improve cohesive teams and communicate better. Their new after-hours action plans to support resilience included opportunities for time-saving people-first items that management could implement. They also took the following steps:
- Improve communication. CHI Health at Home began using technology as a benefit. This includes tactics such as sending out videos and getting information that staff could review on their own time. The goal was to remove burdens that would take attention and time away from their families and off time.
- Improve professional personal balance. Implement flexible work schedules working with individuals that have children, for instance. What does that look like working from this day this time and then coming back to work? They found the “biggest rock” was the external after-hours and weekends on-call. Outsourcing the on-call solution was the most significant adjustment after the analysis.
- Adoption of acute-type flexibility. To attract nurses during the pandemic, CHI Health at Home leaned on their hospital partners to learn what they were doing to attract nurses. Many partners asked the nurses what they wanted to work and adjusted schedules to make that work. 12-hour shifts, 10-hour shifts, split shifts, managing shifts around work in the home, basically altering to an acute setting process.
- Virtual training and virtual visit enhancement. Incorporating technology for remote training and virtual visitation. Telehealth is becoming more common on the home care side. Still, more needs to be talked about virtual visit enhancement in hospice, so CHI Health at Home began looking at that and incorporating that for after-hour solutions and support.
- Shifting non-nurse responsibilities. A good takeaway for CHI Health at Home is what the nurses were doing. Just because nurses can perform a task doesn’t mean they should, so the organization reassigned duties. They also eliminated redundancies in the EMR and centralized visit notes.
- Outsourced after-hours phone triage. The most significant action plan for after-hours was handing our phones to IntellaTriage.
Optimized After-hours Results
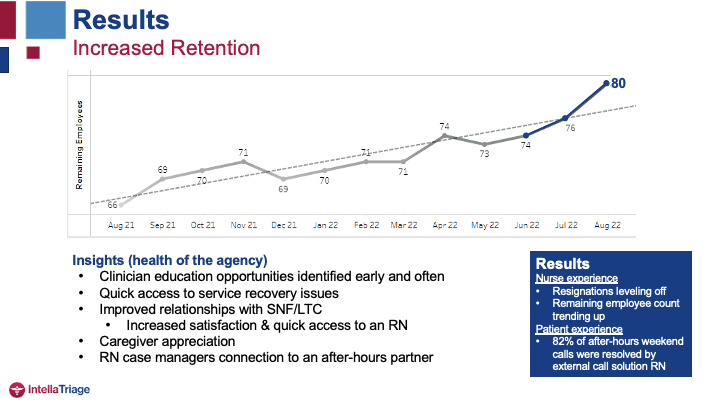
Since IntellaTriage services began in June:
- CHI Health at Home has hired six nurses, which equates to quite a few patients being able to be brought on to service. There are increased visits and improved meeting of the community need.
- Resignations are leveling off, and the new after-hours solution received positive feedback at recent town halls.
- Nurses are telling their friends about it.
- Nurses are reporting feeling personal and professional balance and satisfaction. They enjoy going home to refresh, renew, and re-energize. Then they return the next day to care for their patients and be more available.
There are other positive impacts resulting from the after-hours action plans. CHI Health at Home’s remaining employee count is trending up. External triage nurses resolve 82% of the after-hour weekend calls, which offloads the nurse. Unlike home health, hospice COPs state that a nurse must be available to visit after hours. Still, nurses have experienced a significant decrease in calls so that they can sleep more extended periods after hours and at night. Nurses are confident the phones are being answered when they are on a visit or are at a death visit. There is a reported sense of support in the after-hour partner.
“We are working on layering people in, but knowing that the patients are calling and getting an RN right away, it has been a great relief to our weekend staff.” – L. Schmitz.
Call wait times with IntellaTriage are down into the seconds: thirty-two seconds wait time. It is a considerable departure from the previous process. That process included a call tree and leaving a message, and often could take up to twenty minutes to contact a nurse. Shortened wait times positively impact the caregivers as well. It’s scary at 2-3 in the morning when something’s going differently than at 8 or 9 at night. So, the caregiver’s ability to immediately reach an RN who can help them through whatever crisis or situation is essential to call out. It makes you a vital partner with your long-term care individuals and patients’ families.
More about IntellaTriage
At IntellaTriage, our nurse-based triage can reduce nurse burnout and staff turnover, improve patient satisfaction, and boost your bottom line. You can save on the cost of staffing an internal call center and the time and effort of recruiting, managing, and operating that service. We capture all referrals quickly, increasing your topline revenue and your patient’s healthcare outcomes.
Contact us today to learn more about IntellaTriage’s revolutionary approach to nurse-based triage service.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
Post-acute triage call volumes continue to rise across hospice and home health, driven by higher census, caregiver anxiety, increased acuity at home, and symptom flare-ups. Field nurses are stretched thin, documentation requirements increase regularly, and families expect and deserve immediate clinical guidance, not voicemail. The confluence of these factors mean agencies are paying closer attention [...]
In 2025, post-acute care entered a new era of accountability and transformation. Hospice and home health providers faced the rollout of new quality measures, mounting documentation demands, and continued pressure from shrinking margins and workforce shortages. Families expected faster access and more compassionate communication, while clinicians needed real relief from after-hours strain. At the same [...]
For hospice and home-health organizations, staffing after-hours shifts presents a unique challenge. Patients’ needs don’t magically pause between office hours, yet many agencies still rely on outdated scheduling models that leave nurses exhausted, escalation rates high, and patient satisfaction vulnerable. In this post, we’ll explore how thoughtful scheduling, strategic outsourcing, and nurse-first triage support can [...]