Burnout in healthcare is a real concern of today’s providers; the areas of hospice and post-acute care are no exception. It’s costly, on a human and a financial level and it can negatively impact patient experience and outcomes. Enlisting the help of an after-hours triage service can give providers a way to reduce these issues and, in turn, provide benefits to not only the agency but to the client and their patients as well.
The Nursing Shortage
According to a 2020 survey, hospice leaders worry more about staffing concerns than the growing competition and new payment models. And for a good reason: the 2020-2021 turnover rate for hospice nurses is 22.8%. The American Nurses Association predicts that more open nursing positions will be open than any other profession in the United States through 2022. Posing the question: how can hospice organizations improve nurse job satisfaction, patient experience, and cost-savings?
More than ever, hospice agencies must find ways to attract and retain top nursing talent. One way to do that is to address the common issue of nurse burnout.
Causes of Hospice Nurse Burnout and Turnover
Hospice nursing is both meaningful and demanding work. While many hospice nurses find caring for patients and their families to be rewarding, studies show that hospice nurses experience significant professional burnout. These nurses see death and grief more often throughout their careers than most do in a lifetime, but studies show that this is not typically the primary cause of chronic workplace stress. In fact, workload and administrative demands contribute more to hospice worker burnout than witnessing dying and death. The top challenges of the profession are the heavy workload, administrative demands, witnessing loss and grief, difficulty taking time off, maintaining work-life balance, and unpredictable schedules.
ChronChronic workplace stress is also a physiological weight that can often be found in nurses, particularly those who also work on-call and is a leading cause of burnout. It can manifest itself in physical and emotional exhaustion, absenteeism, worsening work performance and retention problems.
Partnering with an After-Hours Nurse Triage Service
The key to addressing nurse burnout and turnover is improving the quality of life for hospice nurses. A consistent stressor for hospice field nurses is the volume of calls they receive after hours from caregivers of hospice patients looking for emotional support, symptom management guidance, and caregiving tools, such as durable medical supplies or medication refills.
All of these tasks can easily be handled by a nurse-based triage service. This additional layer of support improves the nurse’s quality of life and the care they can provide.
For most hospice agencies, outsourcing a nurse-based, after-hours triage service is more cost-effective and efficient than handling after-hours calls in-house. By partnering with a reputable triage service, you can reduce burnout and turnover in your nursing workforce, improve patient and caregiver satisfaction and realize cost savings.
Download the full report for key criteria to consider when determining your after-hours staffing model.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
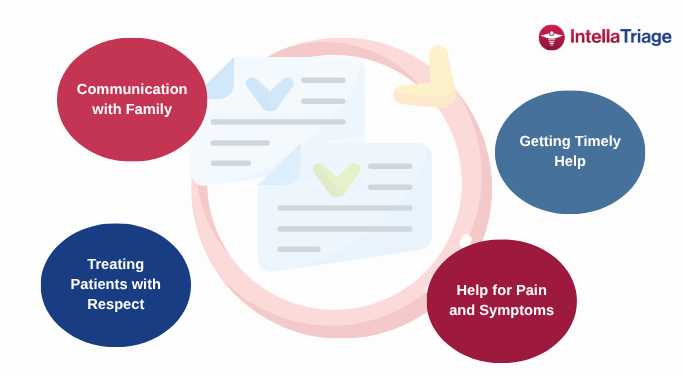
People who work in hospice care understand that, at its core, it is the lived experience of patients and their families during some of life's most vulnerable moments. As regulatory expectations rise and patient-centered care becomes the standard, hospice providers should proactively influence the quality measures that shape outcomes, perceptions, and reimbursement. Key hospice quality [...]
Our recent post, Thinking Outside the QAPI Checkbox, explored how utilizing QAPI as a proactive, clinician- and patient-driven process leads to more meaningful improvement. Today, we are taking that idea further, illustrating the real-world impact of what happens when we drive seamless communication, take action on data, and implement structured after-hours nurse triage programs. A [...]
Patient experience is a leading indicator of clinical outcomes. Full stop. Hospice and home health providers, especially quality leaders at those organizations, often find themselves caught in the traditional check-a-box QAPI cycle: identify a quality issue, create a corrective plan, and check a box. However, reframing QAPI as an opportunity for proactive improvement (not just [...]