On the IntellaTriage blog, we’ve explained exactly how detrimental nurse burnout can be to your organization and your team. When staff members are pushed to the limit, they begin to feel stressed, anxious, and fatigued. This often results in issues with nurse retention and recruitment, with the average cost of turnover per employee reaching up to $58,400. Today, we’d like to shed light on another major concern: the relationship between nurse burnout and patient safety.
How Nurse Burnout Impacts Your RNs and LPNs
The pandemic has pushed nurse burnout into overdrive. For many healthcare workers, the trauma and long hours required due to COVID have caused them to become overwhelmed. They then face a difficult choice: Do they persevere or find a new line of employment?
In an interview with NBC News, Colorado nurse Joanna Engman said,
“You’re seeing someone who is scared and suffering, and you’re not able to be present with them because you’re so overworked. The hardest part for me was feeling like I had no support. There was no one [hospital nurses] could speak to, and our mental well-being was beginning to deteriorate.”
After more than a decade in the field, Engman chose to leave in February of this year. When you consider the issues that she and other nurses face, it’s no surprise that many have made the decision to seek new opportunities. Overnight shifts, staff shortages, responsibility overload, feelings of hopelessness, high-stress environments, and bullying from coworkers or patients all contribute to increasing levels of nurse burnout.
Ultimately, burnout has the following effects on nursing staff:
- Near-constant fatigue or exhaustion
- Disruption of sleep schedule
- Poor attitude about work, dreading shifts
- Loss of appetite
- Higher rates of depression and anxiety
- Inability to pay attention or concentrate on tasks
- Compassion fatigue (inability to empathize with patients)
The list above illustrates exactly why this phenomenon poses an incredible threat to patient safety.
Burnout Jeopardizes Patient Safety
In her NBC interview, Joanna Engman also explained the dangers of emotional and physical exhaustion among healthcare workers. “A burned-out nurse is a dangerous nurse. An exhausted nurse is not a safe nurse. Unless there are tangible changes, we’re going to see this get worse.”
Research backs up her claims. In a 2010 study from the Canadian Nurses Association and the Registered Nurses’ Association of Ontario, psychologists found that nurse fatigue has been linked to serious (and potentially fatal) mistakes in patient care. It’s important to note that this research was truly extensive, with a sample size of more than 7,000. Therefore, it is safe to assume that it is representative of the issues faced by healthcare workers.
Errors that threaten patient safety include:
- Mistakes when updating patient charts
- Administering incorrect dosages of medication
- Incorrect assessment of the patient
- Slowed reaction time
- Unclear communication
- Indifference, loss of empathy
- Failure to rescue patients
- Increased errors of omission
- Misunderstanding patient needs
- Giving patients the wrong medication
- Irritability and tenseness
- Irregular monitoring
- Increased errors in the performance of repetitive tasks
- Falling asleep on duty
- Compromised ability to problem-solve
- Absenteeism (calling out of work)
- Increased risk of falls and injury
The researchers observed that even though most healthcare workers understood that exhaustion could affect quality of care, they tended to think that they were exempt from its effects. This attitude – “it could never happen to me” – contributes to errors that verge on the unbelievable. The Canadian agencies found cases of nurses caring for the wrong patient, choosing the incorrect implants for procedures, and being unable to focus while counting. Fortunately, there are steps healthcare leaders can take to improve conditions in their facilities.
Protection for Patients and Nursing Staff
Clearly, there is a strong correlation between nurse burnout and patient safety. When healthcare providers are unable to recover from long shifts and ongoing stress, lives are on the line. It has become imperative for administrators to mitigate the effects of fatigue among nursing staff. Here are a few of our recommendations for doing just that.
Flexible Scheduling
Half of nurses surveyed said that they missed scheduled shifts due to fatigue; for some, this happened every other month. Older nurses are especially vulnerable to this. Studies indicate that variable scheduling could help staff to establish healthy circadian rhythms and become fully rested between shifts.
Addressing the Five Factors Behind Burnout
The top issues that contribute to burnout are increased workload, high expectations, staff shortages, disorganized workplaces, and unexpected emergencies. While some of these circumstances, like emergencies, will always be common in a clinical setting, leadership should take steps to address the factors within their control.
Uninterrupted Time Off
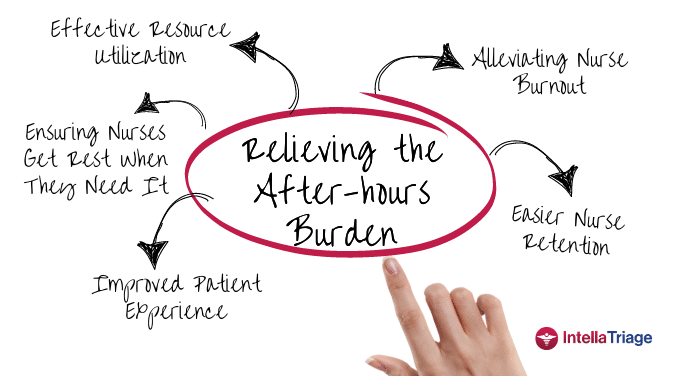
An estimated 29% of nurses worked “on-call” for up to seventy hours each week. Around one third of them chose this duty, while some said they were simply “on-call all the time.” This constant state of alertness prevents workers from fully relaxing even while they’re at home. For this reason, “on-call” nursing is a chief contributor to the patient safety errors mentioned above.
Services like IntellaTriage can take on the responsibilities of on-call nursing staff. Our network of registered nurses provides first-class medical support to all patients. They also update the electronic medical records after every conversation, ensuring that you are aware of what transpired during that interaction.
Integrating IntellaTriage into your hospice, hospital, practice, or home health agency allows your nurses to take care of their patients and themselves. To learn more, please contact us online.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
Burnout among healthcare professionals, particularly nurses, is a persistent issue. The ongoing nursing shortage and the upcoming boom in the aging population have intensified this problem, adding urgency to hospice and home health organizations' efforts to find effective solutions. While traditional methods focus on workload and administrative burdens, innovative strategies address the root causes of [...]
In a recent milestone, IntellaTriage and CommonSpirit Health at Home (CSHaH) announced a significant integration between IntellaTriage’s IntellaHub and CSHaH's electronic medical records system, Homecare Homebase. This partnership underscores the importance of interoperability in healthcare, particularly in post-acute settings like hospice and home healthcare. Here are the top five reasons why interoperability is essential in [...]
Preventing nurse burnout can translate to improved nurse retention and improved patient outcomes. In home health and hospice care, nurses often face significant challenges that can lead to burnout. The constant juggling of patient needs, administrative tasks, and emotional stress can take a toll on even the most dedicated caregivers. However, prioritizing nurse wellness and [...]