We’ve previously discussed the impact that burnout can have on men and women in the health care field. Today, we want to talk about a principal factor behind that stress and exhaustion: compassion fatigue. What is this phenomenon, and how can employers protect their staff from nursing burnout?
Emotional Exhaustion in the Nursing Profession
The health care environment fosters burnout unlike any other. Demanding shifts, significant staffing shortages, and uneven patient assignments all contribute to the pressure felt by caregivers. While recharging at home can help, that’s not always accessible. Many nurses become burnt out by fielding calls after hours. However, there is another factor at play which is unique to the health care profession.
In this blog post, we want to discuss the emotional exhaustion created by the day-to-day stressors of working in a medical setting. This applies to nurses of all levels who work in hospice, home health, hospitals, or private clinics – any area in which face-to-face patient care is required.
The American Psychological Association defines compassion fatigue as a numbness to patients’ suffering. After interacting with hundreds of patients, many of whom present with serious health concerns, some nurses lose the ability to empathize or relate to their patients. This serves as a sort of “shield” to protect nurses from suffering alongside those in their care. Some researchers call it “a stress reaction” that serves to insulate hospital staff from vicarious trauma.
Some examples of triggers for compassion fatigue include:
- Providing care in a dangerous setting (COVID-19 wards, for example)
- Being abused, verbally or physically, while providing care
- Specializing in care for those at the end of their lives
- Being threatened by patients
- Caring for the vulnerable, such as children or the elderly
- Treating patients with severe mental illness (depression, suicidality)
- Experiencing multiple patient deaths
Compassion Fatigue Symptoms
This condition can impact patient care and affect nurses’ ability to function at home and at work. Luckily, there are clear signs of compassion fatigue. With quick and proper intervention, it is possible to treat this type of apathy, resulting in better outcomes for staff and patients alike.
Signs of compassion fatigue:
- Drastic mood swings
- Pessimism and cynicism
- Irritability or a short temper
- Detachment
- Headaches
- Digestive issues
- Addiction (self-medication or addictive behaviors)
- Inability to concentrate or remember things
- Insomnia and exhaustion
- Anxiety and depression
- Changes in appetite
Compassion Fatigue Test
If you believe that a member of your staff may be suffering from compassion fatigue, we invite you to give them the quiz below.
- Do your personal issues often interfere with your role at work?
- Do you believe that friends, family members, and other nurses lack understanding?
- Do you find changes – even small ones – to be draining?
- Do you find it difficult to recover quickly after a troubling event?
- Are you deeply affected by trauma or negative events?
- Does the stress of your patients affect you deeply?
- Have you lost your feelings of hopefulness?
- Do you feel vulnerable at all times?
- Do you feel overwhelmed?
If members of your nursing staff answered “yes” to more than two of these questions, it is time to take additional measures.
Help for Nurses
Nurses can incorporate many healthy practices into their daily lives that will improve their compassion fatigue over time. These include meditation, self-care, more flexible scheduling, and taking vacations. However, there are also steps that employers should take to alleviate the stress felt by nursing staff.
Nursing burnout – the feeling of detachment and resentment that comes from a demanding career – often follows the presentation of compassion fatigue symptoms. To avoid dealing with both concerns at once, we recommend that hospital leadership, clinicians, and other health care employers take a proactive approach to stress relief in the medical field.
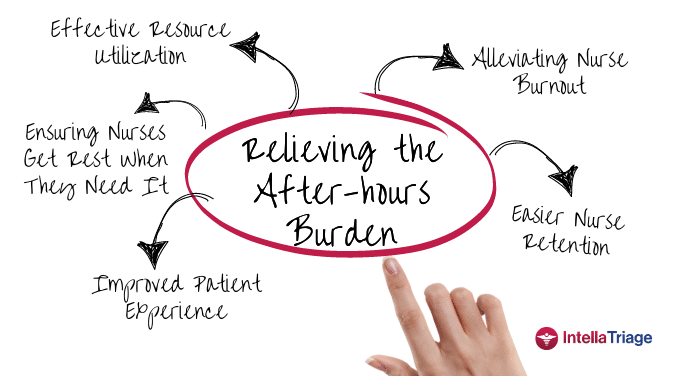
IntellaTriage offers an innovative tool for the prevention of nursing burnout. We are available to field patient calls 24/7. This means that your nurses won’t have to step away from patients to answer questions. They also won’t be called after hours, meaning that they can fully enjoy that restorative time outside of work. All told, this significantly reduces the stress felt by nurses in home health, hospice, and other clinical settings. It also gives them the freedom to relax and process the day’s events in the privacy of their own homes, freeing up hours that would have otherwise be spent “on call.” This healthy separation empowers each nurse to address compassion fatigue, care for themselves and their families, and arrive fully rested for their next shift.
We understand that you want to provide top-notch care at all hours of the day. That’s why all your calls will be answered by highly qualified registered nurses (RNs). Whether your patient is seeking advice about their medication or triaging new symptoms, our licensed staff will walk them through the best next steps. IntellaTriage also integrates with your EMR systems; our staff will take extensive notes so that your practice is aware of each and every call.
Experience the IntellaTriage Difference
You care about your nurses, your patients, and your quality of care. IntellaTriage will serve as your partner, providing excellent outcomes in each of these areas. To learn more about our service, submit a contact form. We look forward to speaking with you.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
Burnout among healthcare professionals, particularly nurses, is a persistent issue. The ongoing nursing shortage and the upcoming boom in the aging population have intensified this problem, adding urgency to hospice and home health organizations' efforts to find effective solutions. While traditional methods focus on workload and administrative burdens, innovative strategies address the root causes of [...]
In a recent milestone, IntellaTriage and CommonSpirit Health at Home (CSHaH) announced a significant integration between IntellaTriage’s IntellaHub and CSHaH's electronic medical records system, Homecare Homebase. This partnership underscores the importance of interoperability in healthcare, particularly in post-acute settings like hospice and home healthcare. Here are the top five reasons why interoperability is essential in [...]
Preventing nurse burnout can translate to improved nurse retention and improved patient outcomes. In home health and hospice care, nurses often face significant challenges that can lead to burnout. The constant juggling of patient needs, administrative tasks, and emotional stress can take a toll on even the most dedicated caregivers. However, prioritizing nurse wellness and [...]