The Role After-Hours Plays in the Emotional Experience of Nurses, Patients, and Family Members
For home and community-based services, patients’ healthcare needs do not go on pause when the office doors close and the phones are “off” for the night. In fact, during those roughly 126 hours, organizations can expect call volumes as high as 65-75% of their daily census in call volume. Have you ever been put on hold or spent ages pressing buttons trying to get an actual human being on the phone? Then, you can relate to the frustration and aggravation that results from having no one to speak to. Now consider how intense that feeling would become when a loved one in hospice experiences a change in condition or a home health patient realizes their medication has run out and the office is closed for two days.
Having a medical question or concern overnight is scary and often compounded by feeling isolated and overwhelmed. No one wants to speak with their healthcare provider after hours. Chances are, if a patient or caregiver was concerned enough to place the call, they need emotional support and reassurance – even if, on the surface, it appears to be a call about scheduling. Access to a nurse on the phone during after-hours can significantly reduce anxiety, provide emotional support, and decrease hospitalizations and urgent care visits. IntellaTriage understands this vulnerability and equips nurses to offer medical advice and empathy, ensuring patients and caregivers feel supported until morning.
The Emotional Experience of Patients and Caregivers During After-Hours
Patients often feel vulnerability and fear overnight due to the unavailability of their healthcare staff. Direct access to an experienced nurse can lessen anxiety, reduce the sense of urgency surrounding a situation, and reduce hospitalizations and urgent care visits. Nurses can educate the caller about their concerns, offer emotional support and medical advice, and refill a prescription or advise on medication to help the caller feel supported and cared for until morning. Simply providing empathy and an ear to listen versus passing along a message can diffuse the situation. At IntellaTriage, our nurses have access to the patient’s record, with a direct line of sight into the patient’s current status and diagnosis, able to address patient anxieties and concerns during after-hours.
Family members and caregivers also experience this vulnerability during after-hours. Care often rotates among family members, and the education one caregiver receives is not always accurately passed along to the next person “on shift.” Communication can be incorrect, incomplete, or nonexistent, causing anxiety and confusion. These feelings often increase overnight and on weekends when caregivers feel they do not have access to a clinician for information. Particularly in hospice, an already emotional time, having limited access to clinicians can feel challenging.
For both the patient and the caregivers, accessibility to after-hours care and reducing anxiety during those times has been shown to improve their overall experience and outcomes measures in home health and enhance the patient experience in hospice. Overall, nurses and patients as a unit report better satisfaction and reduced anxiety, resulting in better care and experiences. While patient experience is an essential consideration in and of itself, this metric is also associated with crucial clinical processes and outcomes. For example, patients with diabetes have demonstrated more effective self-management skills and improved quality of life after reporting more positive interactions with their healthcare providers. Put simply, when you invest in aftercare, you can change a patient’s outcome.
The Emotional Experience of Nurses During After-Hours
A typical after-hours staffing structure includes having nurses available to triage calls and make home visits after hours. Often, these nurses have completed a full day’s work and rotate this on-call shift weekly. They are tired from their day shift and must remain alert, waiting for calls throughout the night. There is no proper rest time, and they return to work tired and less likely to perform their best the next day. For hospice nurses, the stress of this overnight on-call cycle is compounded by compassion fatigue. Rotating on-call nurse schedules results in high nurse turnover and burnout. In fact, on-call ranks in the top three of employee dissatisfiers in home health and hospice nurses and is blamed for reduced or nonexistent work-life balance, a crucial element in reducing nurse burnout and improving job satisfaction and nurse performance.
Strategies for Improving the Emotional Experience During After-Hours
IntellaTriage provides a holistic solution for improving the emotional experience for nurses, patients, and caregivers after hours.
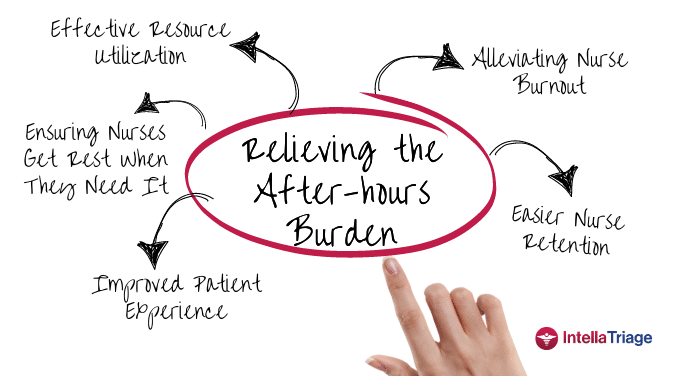
Enhancing the Nurse Experience. Outsourcing triage helps reduce burnout by alleviating much of the after-hours burden – and can eliminate it for home health. With nurse-first triage, triage nurses become field nurses’ first line of defense. Nurses report feeling less overwhelmed by phone calls while trying to care for patients and performing all the other duties they face during their workday. When professional triage nurses address your organization’s after-hours patient calls, your nursing staff will experience:
- Increased rest and recovery between shifts.
- Reduced extended hours and an improved workload.
- Relieved burnout-associated symptoms such as fatigue and reduced enthusiasm.
Enhancing the Patient Experience. The answering service model needs to serve the patient and the nurse better. The triage model flips that on its head by integrating emotional support services and clinical advice as part of after-hours care. In fact, in under 60 seconds, on average, you have a nurse answering the phone who is hospice trained, has hospice experience, and has the EMR open in front of them with the medication profile. The triage nurse has the Plan of Care, the notes that the case manager entered at 7:00 PM that night, etc. That nurse can walk through the situation with the caller, provide emotional support, and decide whether or not a visit needs to be made.
Enhancing Communication Between Nurses, Patients, and Family Members. Effective communication is also vital within your team. Services like IntellaTriage provide customized aftercare for your patients and deliver patient feedback to your practice. For example, call notes are entered directly into your EMR, and items requiring physician attention are flagged for review. When these interactions are regularly logged, everyone on the healthcare team can improve their patient care and communication, as well as the patient’s health outcomes.
External Triage Recognizes After-Hours is Way More Than Just a Phone Call
At IntellaTriage, we know that when a patient or caregiver calls after-hours, they need more than an answering service on the other line. We tailor after-hours solutions to meet the needs of your facility, staff, and patients. All calls are answered in an average of 60 seconds or less by a registered nurse with hospice field experience. Our approach is purposefully unique. We believe patients and caregivers should speak to a licensed, registered nurse with hospice field expertise anytime – day or night. As an extension of your team, your patients receive the highest quality of care around the clock. The end result is improved patient satisfaction, reduced nurse burnout and staff turnover, and boosted bottom line.
Contact us today to learn more about IntellaTriage’s revolutionary approach to nurse triage service.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
Burnout among healthcare professionals, particularly nurses, is a persistent issue. The ongoing nursing shortage and the upcoming boom in the aging population have intensified this problem, adding urgency to hospice and home health organizations' efforts to find effective solutions. While traditional methods focus on workload and administrative burdens, innovative strategies address the root causes of [...]
In a recent milestone, IntellaTriage and CommonSpirit Health at Home (CSHaH) announced a significant integration between IntellaTriage’s IntellaHub and CSHaH's electronic medical records system, Homecare Homebase. This partnership underscores the importance of interoperability in healthcare, particularly in post-acute settings like hospice and home healthcare. Here are the top five reasons why interoperability is essential in [...]
Preventing nurse burnout can translate to improved nurse retention and improved patient outcomes. In home health and hospice care, nurses often face significant challenges that can lead to burnout. The constant juggling of patient needs, administrative tasks, and emotional stress can take a toll on even the most dedicated caregivers. However, prioritizing nurse wellness and [...]