While burnout in the healthcare field is not a new concept, the historic staff shortages brought on COVID-19- related burnout has launched it into the spotlight. There are a number of specific reasons for the high burnout rate, even during “normal” times. There are also a number of ways to reduce nurse burnout in post-acute care, including enlisting the help of a professional service to take on many administrative and triage duties.
Burnout Rates
According to a 2020 survey, hospice leaders worry more about staffing concerns than the growing competition and new payment models. And for a good reason: the 2020-2021 turnover rate for hospice nurses is 22.8%. This study also found that workload and administrative demands contributed more to hospice worker burnout than witnessing dying and death. In fact, workload and staffing ratios are among the top 10 reasons nurses leave organizations. Even worse, burnout can be cyclical: burnout leads to staff shortages and staff shortages lead to burnout.
Now, more than ever, hospice agencies must find ways to attract and retain top nursing talent, and the way to do that is to address nurse burnout.
Symptoms of Burnout
When a nurse begins to experience the symptoms of burnout, it can affect the quality of patient care they’re able to provide as well as the nurse’s own mental and physical health. Common warning signs of nurse burnout can include:
- Constant Fatigue. When a good night’s sleep does not alleviate that tired feeling that comes from a hard day’s work, it can be a sign of physical exhaustion, an early sign of burnout.
- Feeling Overworked or Under-Appreciated. Nurses often feel as though their hard work goes unnoticed. This can lead to a sense of being burned out with the job. Nurses who work excessive hours or who are not given the support or resources they need may begin to feel this way.
- Lack of Enthusiasm about Work. When a nurse is no longer passionate about the job, but instead is just going through the motions, that is also a symptom of burnout. Dreading going to work or only being able to think about leaving work can be detrimental to patient care. The stress and lack of enthusiasm can also impact many other areas of the nurse’s life.
- Compassion Fatigue. The emotional stress of the job can lead to a loss of compassion and a sense of detachment from patients. The nurse may become cynical about the job or even feel like they are failing in their work. This burnout symptom can also seriously affect patient health as well as the nurse’s mental and physical health.
Doing More with Less
A large part of the reason for their burnout, nurses say, is that they are expected to do more with fewer resources available to them. With the demand for nurses predicted to increase by 15% by 2026 and the fact that there is a direct link between nurse engagement and patients having better experiences, reducing nurse burnout in post-acute care is critical for healthcare providers. The report cited factors such as staffing and resources, leadership responsiveness and teamwork and collaboration as being important in the initiative to engage nurses to restore their joy and purpose more fully.
Help for Healthcare Organizations
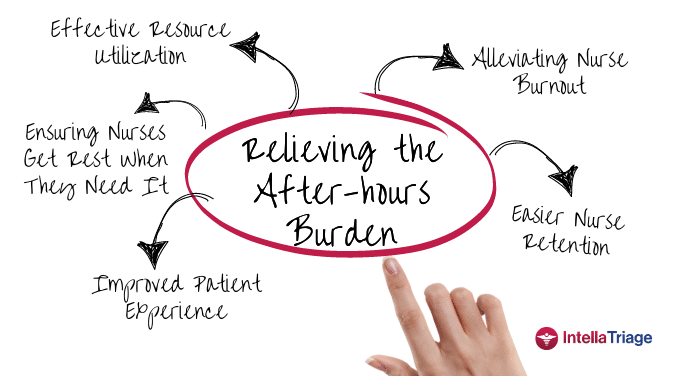
An incredibly beneficial way to reduce nurse burnout in post-acute care is to enlist the services of a professional nurse triage team. These teams comprise licensed nurses with years of experience in hospice care. They can address a large percentage of your organization’s after-hours patient calls, allowing your on-call staff to gain much-needed rest and recuperation. When a nurse is not overwhelmed by phone calls while trying to care for patients and perform all the other duties they face within their workday, they are less stressed. Adding this level of support can also be a way to acknowledge and address other symptoms of burnout, such as feeling overworked and under-appreciated.
As the demand for skilled nurses continues to grow, the duties of a nurse will expand to include training other nurses. When the responsibilities of answering the phone, training others on answering phones and staffing an advice line are removed from the duties of an already overburdened nurse, the possibility of burnout decreases significantly.
Extended hours are also reduced for the organization’s nursing staff with a nurse triage service. The burnout symptoms of fatigue and reduced enthusiasm can be reduced with reasonable work hours and a manageable workload. These are all possible with a nurse triage service.
Reduce Your Team’s Post-Acute Care Burnout
At IntellaTriage, we can reduce nurse burnout and staff turnover, improve patient satisfaction and boost your bottom line. You can save on the cost of staffing your own nurses for an internal call center, as well as the time and effort needed to recruit, hire, manage and operate that service. We also capture all referrals quickly, increasing your topline revenue and your patient’s healthcare outcomes.
To learn more about IntellaTriage’s revolutionary approach to nurse triage service, contact us today.
Contact Us for a Consultation
Ready to optimize your triage process? Reach out to us today for a consultation tailored to your needs. Let’s elevate your patient care together.
More From The Blog
Burnout among healthcare professionals, particularly nurses, is a persistent issue. The ongoing nursing shortage and the upcoming boom in the aging population have intensified this problem, adding urgency to hospice and home health organizations' efforts to find effective solutions. While traditional methods focus on workload and administrative burdens, innovative strategies address the root causes of [...]
In a recent milestone, IntellaTriage and CommonSpirit Health at Home (CSHaH) announced a significant integration between IntellaTriage’s IntellaHub and CSHaH's electronic medical records system, Homecare Homebase. This partnership underscores the importance of interoperability in healthcare, particularly in post-acute settings like hospice and home healthcare. Here are the top five reasons why interoperability is essential in [...]
Preventing nurse burnout can translate to improved nurse retention and improved patient outcomes. In home health and hospice care, nurses often face significant challenges that can lead to burnout. The constant juggling of patient needs, administrative tasks, and emotional stress can take a toll on even the most dedicated caregivers. However, prioritizing nurse wellness and [...]